By Megan DeMott, Occupational Therapist And Girlfriend to A Quadriplegic
Proper positioning in the chair, weight shifting, and pressure sores/marks, do you know anything about this? If you already know this information, this blog will be a reminder and if you don’t this information can help prevent one of the most severe conditions that can slowly or quickly arise even for those people in the best seating equipment.
As an Occupational Therapist, there are many things that I assess that contributes to a person’s quality of life. For women whose significant others are using a wheelchair as their primary means of mobility, this article is a vital way to help prevent pressure injuries. Your significant other’s bones of the hip and spine bear the upper body weight for anywhere from 8-12 hours a day. That being said, seating and positioning are among the most critical concerns due to the medical complications of skin ulceration that can arise from not being in the proper position and or with prolonged static non-shifting sitting time. The incidence of pressure ulcers in the SCI population is 25–66% (Kruger et al., 2013).
The complications are related to seating design and positioning that you can identify include but are not limited to progressing stages. SO, the early identification of those signs and symptoms of tissue change are paramount.
The key things to look at and steps to take if you think your loved one has a pressure injury are presented in stages. The stages format are for your information, but importantly what you see at the superficial skin level indicate that tissue changes are occurring within.
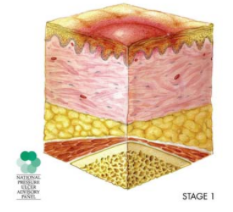
Stage #1:
Signs: The skin is not broken like you would see with an open sore, but is red or discolored or may show changes in hardness or temperature compared to surrounding areas. When you press on the area, it stays red and does not lighten or turn white (blanch). The redness or change in color does not fade within 30 minutes of observation and pressure removal.
What to do: Stay off the area and remove all pressure; keep the area clean and dry; eat adequate calories high in protein, vitamins (especially A and C) and minerals (especially iron and zinc); drink more water; find and remove the cause; inspect the area at least twice a day; call their healthcare provider if it has not gone away in 2-3 days.
Healing time: A pressure sore at this stage can be reversed in about three days if all pressure is taken off the site.
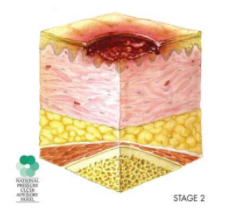
Stage #2
Signs: The topmost layer of skin (epidermis) is broken, creating a shallow open sore. The second layer of skin (dermis) may also be broken. Drainage (pus) or fluid leakage may or may not be present.
What to do: Get the pressure off, follow steps in Stage 1, and see their healthcare provider right away.
Healing time: Three days to three weeks.
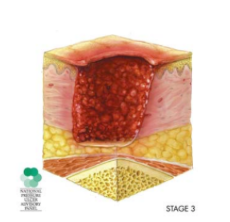
Stage #3
Signs: The wound extends through the dermis (second layer of skin) into the fatty subcutaneous (below the skin) tissue. Bone, tendon and muscle are not visible. Look for signs of infection (redness around the edge of the sore, pus, odor, fever, or greenish drainage from the sore) and possible necrosis (black, dead tissue).
What to do: If you have not already done so, get the pressure off and have your partner see their health-care provider right away. Wounds in this stage frequently need special wound care. If your partner has had this stage of injury they may also qualify for a special bed or pressure-relieving mattress that can be ordered by your health-care provider.
Healing time: One to four months.
Stage #4
Signs: The wound extends into the muscle and can extend as far down as the bone. Usually lots of dead tissue and drainage are present. There is a high possibility of infection.
What to do: Always consult your health care provider right away. Surgery is frequently required for this type of wound.
Healing time: Anywhere from three months to two years.
In summary, if you are concerned about your significant other developing a pressure injury these are the signs and symptoms.
- First Sign: reddened, discolored or darkened area. It may feel hard (full) and warm to the touch as compared to the surrounding area.
- A pressure sore has begun if you remove pressure from the reddened area for 10 to 30 minutes and the skin color does not return to normal after that time. Have your partner stay off the area. Importantly, the next step is to find and correct the cause immediately. If the tissue responds and you return to the same sitting routine the condition will return.
- Test the suspect skin area with the blanching test, this indicates blood flow to the area.
(Blanching test: Press on the red, pink or darkened area with your finger. The area should go white; remove the pressure and the area should return to red, pink or darkened color within a few seconds, indicating good blood flow. If the area stays white, then blood flow has been impaired and damage has begun)
*Dark skin may not have visible blanching even when healthy, so it is important to look for other signs of damage like color changes, heat or hardness compared to surrounding areas.
Warning… The surface of the pressure injury is often the smallest part. Which can deceive you into thinking they have a only small problem. But damage in the tissues underneath the skin suffers the greatest damage. Skin damage from pressure injury doesn’t start at the skin surface. Every pressure sore seen on the skin, no matter how small, should be regarded as serious because of the probable damage below the skin surface. (SCI Model Systems, et al., 2009)
Specific Steps you and your loved one can take to prevent pressure injuries:
- Regular pressure reliefs. Every 15 to 30 minutes for a duration of at least 30 to 90 seconds.
- Checking skin, if they are able to do it on their own or have a caregiver do it, a minimum of twice a day (morning and bedtime).
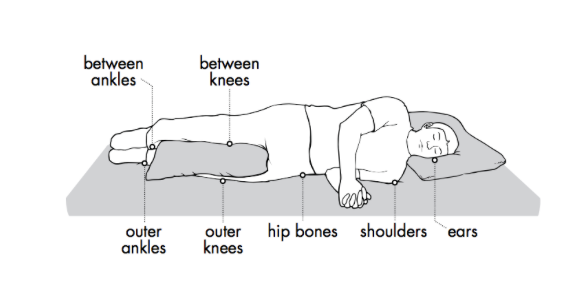
- Padding, positioning and turning in bed.
- Keep skin clean and dry
- Get a proper seating evaluation at least every two years or sooner if your health or skin condition changes.
- Positioning and transferring
- Clothing, shoes
- Wear properly fitted clothing; avoid thick seams, rivets or bulky pockets and check for folds and wrinkles in areas of pressure.
- Hydration
- Nutrition
- Sun exposure - Avoid getting sunburnt
- Equipment
- Temperature
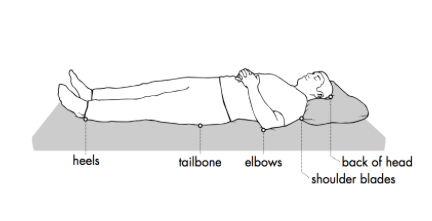
Check your skin in the areas below.
(Craig Hospital Rocky Mountain Spinal Injury System, 2009)
Here is some adaptive equipment your significant other can use to perform their own skin checks:
- Nutrition
- Increase Calories
-
-
- More “healthy” calories should be consumed to meet the increased energy and protein needs necessary for a pressure sore to heal.
-
- Increase Protein
-
-
- Growth and repair of new tissue cannot take place without protein. Studies indicate that low protein levels are associated with both the development of pressure sores and delayed healing.
- Fish (Sardines, tuna, Cod, Haddock, Halibut, & Salmon)
- Beef / Poultry (Beef, Chicken, Eggs and Turkey)
- Beans & Lentils (Quinoa, Chickpeas, Kidney Beans, & Black beans)
- Nuts & Seeds (Almonds, Walnuts, Sunflower Seeds and Pumpkin Seeds)
- Protein Powder (Whey and Collagen Powder) *Easiest way to increase protein by drinking protein shakes.
- Growth and repair of new tissue cannot take place without protein. Studies indicate that low protein levels are associated with both the development of pressure sores and delayed healing.
-
- Vitamin A: Stimulates the growth of the base layer of the skin, maintains skin integrity and promotes wound healing. This vitamin is also needed to enhance the activity of white blood cells and help protect tissues from infections. (Foods High in Vitamin A: sweet potato, kale, spinach, carrots & winter squash)
- Vitamin C: Convert the amino acids proline and lysine into collagen. As well, it also helps the healing process by strengthening the walls of blood vessels. (Foods High in Vitamin C: broccoli, red & green peppers, strawberries, oranges, pineapple, blueberries, raspberries, cherries & papaya.)
- Vitamin D: helps activate T-cells in the immune system to fight infection. (Foods high in vitamin D: sardines, eggs, salmon & cod liver oil)
- Vitamin E: antioxidant that helps stabilize cell membranes, protects tissues and improves circulation. Deficiencies in Vitamin E may contribute to poor wound healing. (Foods high in Vitamin E: sunflower seeds, olives, olive oil, almonds & spinach.)
- Zinc: necessary for cell and tissue formation, skin strength, skin elasticity and repair. (Foods high in zinc: pumpkin seeds, red meat, yogurt, & sesame seeds)
-
-
- Studies suggest that zinc also speeds pressure sore healing and reduces incidence of infection by increasing the production of white blood cells and enhancing their function. Deficiencies in this mineral may lead to tissue breakdown.
-
- Drink 8 Cups of Water / Fluids a Day.
- Water helps your body heal b/c 81% of your blood is water, your blood to carries the necessary repair substances to injury sites.
- Coconut Water:
- Helps your body replenish electrolytes and minerals.
- Take Amino Acids: The following three important for healing process.
- Glutamine
- Helps speed up your bodies natural healing process.
- Lysine
- Building block for protein and helps with collagen formation.
- Proline
- Increases collagen formation.
- Eat Good Fats
- Omega 3 Fatty acids aid with proper cell production & play a role in promoting health in skin.
- Good fats are found in: walnuts, salmon, anchovies, sardines, tuna, halibut, mackerel & ground flax seeds.
- Omega-3 fatty acids can also be taken in supplement form.
- Take Skin Healing Nutrients & Herbs
- Horsetail
- High content of silica, a mineral that helps strengthen tissues, especially skin, hair and nails.
- Co-enzyme Q10 (CoQ10)
- Plays a critical role in circulation, stimulating the immune system, and increasing tissue oxygenation, and it has been shown to help increase healing.
- Methylsulfonylmethane (MSM)
- MSM is a sulfur-containing nutrient which has been shown to accelerate wound healing and reduce inflammation.
(Smith & James, 2013)
***I highly encourage everyone to download this book, it is free from the PVA. It is called Eat Well, Live Well with Spinal Cord Injury by Joanne Smith, BTR Dip, CNP and Kylie James, B.Sc (OT), CNP. Joanne Smith sustained an SCI, herself for about 25 years.
http://www.pva.org/media/pdf/Eat%20Well%20Live%20Well%20with%20Spinal%20Cord%20Injury.pdf
Other holistic methods to help your loved one heal from a pressure injury:
- Essential Oils:
- Lavender, rosemary and myrrh have antibacterial and healing properties.
- Tea tree oil has antimicrobial and antifungal properties.
- Frankincense has the ability to strengthen skin and improve its tone, elasticity, and promotes your bodies natural defense mechanisms against bacteria.
(Mori, et. al., 2016) & (De Rapper, et al., 2013)
- Hydrogen Water Enhances Wound Healing
-
- Hydrogen water intake via tube feeding in elderly patients reduced the wound size of pressure ulcers and enhanced recovery.
(Li, Q., Kato, S., Matsuoka, D., Tanaka, H., & Miwa, N, 2013)
References:
DiGiovine, C. & Koesters, W., (2013). Shoulder Evaluation and Intervention for Manual Wheelchair Users. Lecture presented at Seating Symposium.
Kruger, E. A., Pires, M., Ngann, Y., Sterling, M., & Rubayi, S. (2013). Comprehensive management of pressure ulcers in spinal cord injury: current concepts and future trends. The journal of spinal cord medicine, 36(6), 572-585.
Li, Q., Kato, S., Matsuoka, D., Tanaka, H., & Miwa, N. (2013). Hydrogen water intake via tube-feeding for patients with pressure ulcer and its reconstructive effects on normal human skin cells in vitro. Medical gas research, 3(1), 20.
Pressure Ulcer Stages Revised by National Pressure Ulcer Advisory Panel (2007).
Ryan, J. M. (2006). Teamwork keeps the pressure off: The role of the occupational therapist in the prevention of pressure ulcers. Home Healthcare Now, 24(2), 97-102.
Saint Luke's Health System. (2016). Spinal Cord Injury (SCI) and Pressure Injuries. Retrieved from https://www.saintlukeskc.org/health-library/spinal-cord-injury-sci-and-pressure-injuries
Samruddhi Ghaisas, Elizabeth A. Pyatak, Erna Blanche, Jeanine Blanchard, Florence Clark, PUPS II Study Group; Lifestyle Changes and Pressure Ulcer Prevention in Adults With Spinal Cord Injury in the Pressure Ulcer Prevention Study Lifestyle Intervention. Am J Occup Ther 2014;69(1):6901290020p1-6901290020p10. doi: 10.5014/ajot.2015.012021.
SCI Model Systems, Model Systems Knowledge Translation Center, & Craig Hospital Rocky Mountain Spinal Injury System (RMRSIS). (2009). Skin Care & Pressure Sores Part 3: Recognizing and Treating Pressure Sores https://craighospital.org/uploads/Educational-PDFs/Model-Systems/323.Model-System-See-and-Treat-Pressure-Sores.pdf
SCI Model Systems, Model Systems Knowledge Translation Center, & Craig Hospital Rocky Mountain Spinal Injury System (RMRSIS). (2009). Skin Care & Pressure Sores Part 2: Preventing Pressure Sores. Retrieved from https://craighospital.org/uploads/Educational-PDFs/Model-Systems/322.Model-System-Preventing-Pressure-Sores.pdf
Shepherd Center. (2018). Skin Checks. Retrieved from https://www.myshepherdconnection.org/sci/skin-care/skin-checks.
The National Pressure Ulcer Advisory Panel. (2016). NPUAP Pressure Injury Stages. Retrieved from http://www.npuap.org/resources/educational-and-clinical-resources/npuap-pressure-injury-stages/
Smith, J., & James, K. (2013). Eat Well, Live Well with Spinal Cord Injury. Paralyzed Veterans of America (PVA) Education Foundation.